Sleep test may help diagnose and predict dementia in older adults
Dementia is a growing problem for people as they age, but it often goes undiagnosed. Now investigators at Harvard-affiliated Massachusetts General Hospital (MGH) and Beth Israel Deaconess Medical Center have discovered and validated a marker of dementia that may help clinicians identify patients who have the condition or are at risk of developing it. The findings are published in JAMA Network Open.
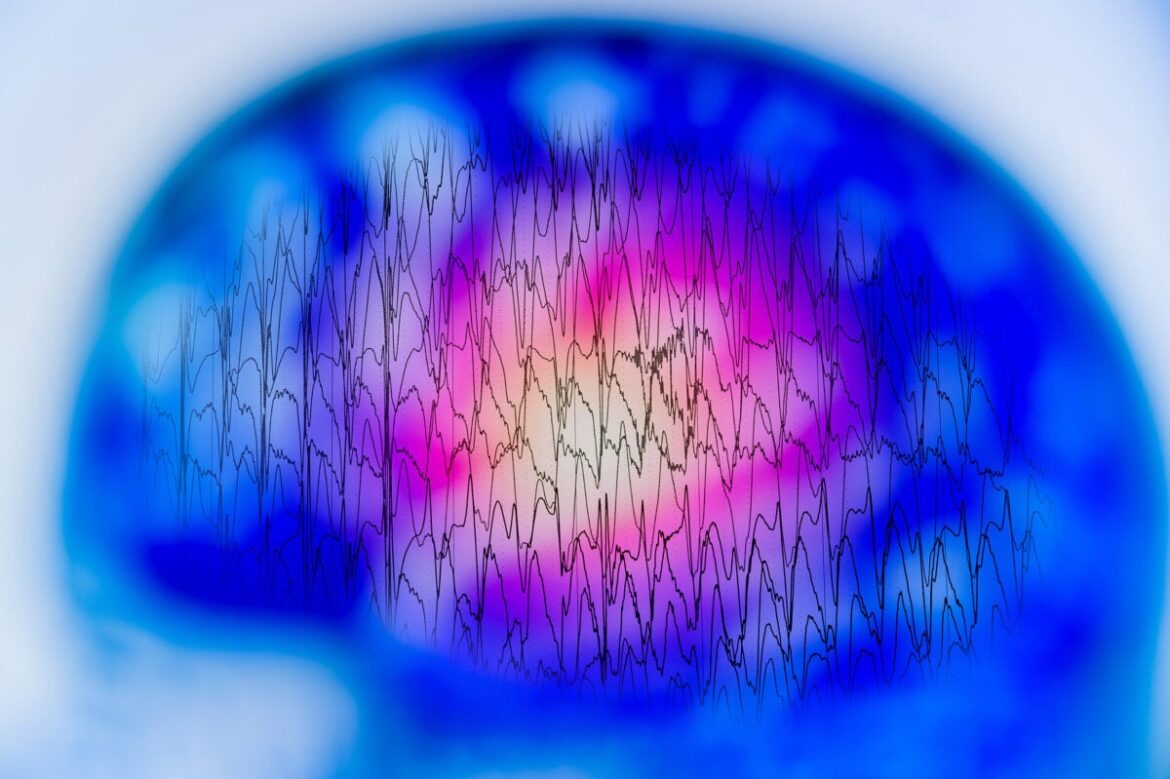
The team recently created the Brain Age Index (BAI), a model that relies on artificial intelligence and a large set of sleep data to estimate the difference between a person’s chronological age and the biological age of their brain when computed through electrical measurements (with an electroencephalogram, or EEG) during sleep. A higher BAI signifies deviation from normal brain aging, which could reflect the presence and severity of dementia.
“The model computes the difference between a person’s chronological age and how old their brain activity during sleep ‘looks,’ to provide an indication of whether a person’s brain is aging faster than is normal,” said senior author M. Brandon Westover, investigator in the Department of Neurology at MGH and director of Data Science at the MGH McCance Center for Brain Health. “This is an important advance, because before now it has only been possible to measure brain age using brain imaging with magnetic resonance imaging, which is much more expensive, not easy to repeat, and impossible to measure at home,” added Elissa Ye, the first author of the study and a member of Westover’s laboratory. She noted that sleep EEG tests are increasingly accessible in non-sleep laboratory environments, using inexpensive technologies such as headbands and dry EEG electrodes.
To test whether high BAI values obtained through EEG measurements may be indicative of dementia, the researchers computed values for 5,144 sleep tests in 88 individuals with dementia, 44 with mild cognitive impairment, 1,075 with cognitive symptoms but no diagnosis of impairment, and 2,336 without dementia. BAI values rose across the groups as cognitive impairment increased, and patients with dementia had an average value of about four years older than those without dementia. BAI values also correlated with neuropsychiatric scores from standard cognitive assessments conducted by clinicians before or after the sleep study.
“Because quite feasible to obtain multiple nights of EEG, even at home, we expect that measuring BAI will one day become a routine part of primary care, as important as measuring blood pressure,” said co-senior author Alice D. Lam, an investigator in the Department of Neurology at MGH. “BAI has potential as a screening tool for the presence of underlying neurodegenerative disease and monitoring of disease progression.”
